Medical Billing Company Services – A Guide To Outsourcing
 You may be considering outsourcing your medical billing to a third party. But what services does a medical billing company offer? Learn more here.
You may be considering outsourcing your medical billing to a third party. But what services does a medical billing company offer? Learn more here.
Healthcare professionals know how complicated medical billing is. And, outsourcing billing seems expensive at first. Though, managing the complexities can cost you money.
If you hire your own staff for billing, you will be responsible for coding and claims. You’ll need a certified medical coder on staff and more personnel to handle rejected claims as well.
Your staff must also keep abreast of changing regulations and new policies. In short, they will wear many hats to manage billing services. Any oversight results in lost revenue.
In this light, hiring a medical billing company could save you more money than it would cost. Want to know more about medical billing services? You’re in the right place.
What Services Does a Medical Billing Company Provide?
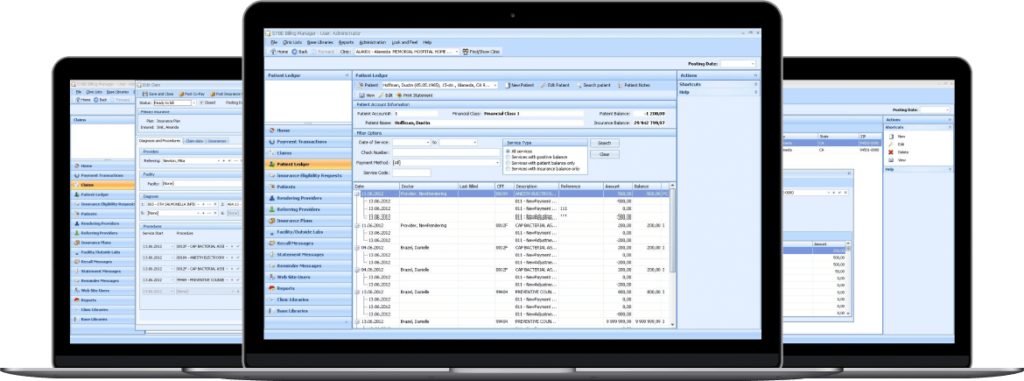
Medical billing companies process and submit health insurance claims. They also follow up on those claims and handle delinquent accounts.
Billing providers train staff to work with individual payers. They use AAPC-certified coders, billing specialists, and accountants.
Managing your revenue cycle means submitting error-free bills and insurance claims on time. Outsourcing coding and billing is the best way to reduce coding and billing errors and improve efficiency.
Medical billing companies handle coding and billing for you. Comprehensive medical billing services cover all the following tasks.
Patient Enrollment
Part of filing reimbursement claims is submitting patient information. Medical billing companies enroll patients using a hospital registration system.
They enter the patients’ demographic and insurance information. This way, insurance companies have the patient data they need.
Insurance Verification and Authorization
Nothing happens until you verify your patients’ eligibility and insurance benefits. Billing companies verify your patients’ active medical coverage. They also check the type of plan and plan exclusions.
They get the claims mailing address as well. They identify patient responsibilities, co-pays, deductible, and co-insurances, if any.
Next, medical billing companies handle the time-consuming task of authorization. The company contacts the insurance company and verify that the insurer will pay for services.
 Coding
Coding
Medical service companies make it a point to perform medical coding with precision. They manage coding audits, DRG/ICD-9-CM coding validations, and CPT coding with accuracy.
Your result is max reimbursement. Coding errors are one of the biggest challenges your in-house billing department has.
Often, such mistakes cost your practice revenue. On the other side, errors cost your patients undue expenses.
Billing and Accounts Reconciliation
Outsourced medical billing focuses on collecting monthly bills. That includes calculating self-accounting totals and handling the transfer of funds for healthcare practices. They concentrate on charge entry, cash posting, and reconciliation.
Accounts Receivable Collections
Medical billing firms handle AR collections, which helps your practice avoid collection issues. They are responsible for patient collection, insurance collection, and AR follow up.
Audit
Billing companies audit charges for accuracy. They ensure the charge team followed proper billing rules. Audits also verify that the claims match carrier requirements.
Why Do I Need Medical Billing Services?
Medical practices choose medical billing outsourcing because it frees up their in-house staff. Though, there are many other benefits to outsourcing medical billing and coding. Here are the top five.
Cost and Convenience
 Billing comes with many direct and indirect costs. Keeping those processes in-house means taking on all those costs, some of which make take you by surprise.
Billing comes with many direct and indirect costs. Keeping those processes in-house means taking on all those costs, some of which make take you by surprise.
Your practice pays a billing provider an agreed-upon fee. There are no surprises, and you can focus on what you do best, concentrate on your patients.
Outsourcing your billing to a medical billing company means they handle the costs. Outsourcing could mean saving thousands of dollars on benefits and salaries.
Not to mention more savings on office furniture and other office supplies. Either way, the cost of paying the billing company is less than what you’d pay to hire, house, and train your staff.
Hardware and Software Upgrades
The software you need to maintain billing, like any software, requires frequent upgrades. You’d also need extra hardware for your billing staff. And that comes with maintenance and upgrade costs.
Outsourcing your billing means avoiding the costs associated with this equipment and software.
Increased Revenue
A medical billing company increases your revenue by reducing lag time for reimbursement. The result is more timely-paid bills. Medical service providers raise the percentage of payments for bills sent.
A medical billing service supports a steady flow of outgoing claims. This results in a steady stream of money coming in. That is the key to maintaining a successful medical practice.
Compliance with Regulations
Medical billing companies are well versed in privacy and HIPAA requirements. They keep up to date with regulation changes as well as the current versions of ICD 10 coding.
This relieves your practice of the burden of compliance. You don’t have to keep training staff to maintain that compliance as it pertains to billing.
Improved Customer Service
Quality patient care must also pair with quality customer service. Trying to balance both can be challenging. Reducing your staff’s load gives your team more time to focus on patients.
This serves to increase patient satisfaction because patient flow improves. Also, a billing company reduces billing errors. Finally, they have dedicated customer service for billing concerns and questions.
 How do Medical Billing Companies Charge Customers?
How do Medical Billing Companies Charge Customers?
Medical billing providers vary their fees based on their clients’ type of practice. Some specialties are more complex. Thus, billing processes take more time.
A billing company charges practices for service in three ways. They can charge by a percentage, per claim, or an hourly rate.
Companies calculate percentage-based fees by the average revenue your practice collects per month. Some companies charge a few dollars per insurance claim filed. Thus, hourly fees make sense for smaller practices.
Last, new clients pay a start-up fee, which could be a few hundred dollars per physician. There is usually a cap for larger practices.
Is It Time to Hire a Medical Billing Service?
Medical billing a coding brings with it layers of regulations and complex processes. Your in-house staff may feel overwhelmed. Is your practice losing revenue due to denied and unpaid claims?
If so, it may be time to consider a medical billing company. Turn your billing and coding responsibilities over to them. A billing service provider speeds up your claims processing and reduces your backlog.
We specialize in reviewing and vetting medical billing service providers. Please contact us for a quick quote on medical billing and coding services.
Author: Mike Cynar
Mike Cynar brings buyers and sellers together by producing reviews and creating non biased webpages allowing users to share their experiences on various products and services. He and his staff write informative articles related to the medical field, legal, and other small business industries.

Leave a Reply