
Mistakes Happen: How to Correct Medical Claims
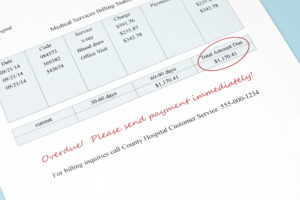
Did you submit a claim that has an error on it? Here’s a quick guide on how to fix medical claims after you’ve submitted them.
Medical billing errors cost Americans roughly $210 billion every year.
Of course, it is important to make sure the medical claims getting sent out are accurate.
Accurate billing ensures quick payment. With that said, mistakes do happen. Clerical mistakes like transposing digits of a CPT, entering demographic information incorrectly, or attaching an incompatible ICD-10 code can easily happen when many claims are being processed.
Here’s what you can do if you receive a claim back that got submitted with an error.
Find the Billing Mistake
The first step is to identify the mistake. A claim can get rejected for a variety of reasons ranging from customer demographic information to incorrect coding.
Insurances will include a reject reason code on the explanation of benefits (EOB). These can sometimes be difficult to decode. Be sure to look up the reason for rejection and examine the claim fully to find the error.

Common reasons for rejections can include duplicate claims, incorrect ICD-10 codes, missing modifiers, and patient eligibility status.
Fix the Insurance Claim
The next step to fix a claim is to correct the error by changing the necessary information. Make sure everything is accurate and double-check that everything gets completed.
At this point, you may want to double-check patient eligibility with the insurance company, demographic information, and whether or not a prior authorization is needed for the service.
Once all the information is correct, it’s time to determine how to resubmit.
Determine the Status of the Claim
If the claim got rejected by a software scrub or before acceptance from the insurance company, the corrected claim could get sent back as if the first try never happened. This type of correction is the easiest and quickest type of correction.
If the claim did reach the insurance company and is being rejected by them, a corrected claim must get submitted. This can get done electronically through your medical billing software, on paper, or through insurance portals.
If the claim got denied, an appeal or re-determination would need to get started. This is much more involved than a corrected claim.
Often, documentation from the visit and re-determination forms must get submitted.
Denials mean that the insurance company saw the claim and decided not to pay the full amount or sometimes decline to pay at all. It is the biller’s responsibility to send any relevant information to support the claim being paid.
Resubmit the Insurance Claim or Re-determination
Depending upon medical billing software capabilities and insurance companies’ requests, claims can be corrected and resubmitted electronically. This is faster and easier; however, paper claims are sometimes necessary.
Alternatively, Medicare has a portal that clerical error re-openings can be submitted. The claim can be corrected on the portal, and a reopening can be initiated.
Paper corrected claims can be printed and mailed to the insurance company with a cover sheet explaining the changes.

The submission must show it is a corrected claim regardless of the delivery method. This will ensure you don’t lose any more time and the claim is not seen as a duplicate.
If a corrected claim is not appropriate and a re-determination or appeal must be done, send in all relevant documentation and the appeal or re-determination form.
Again, the delivery method will depend upon the insurance company. Portals exist on some insurance websites in which documentation can be uploaded.
Paper re-determinations can also be sent through the mail. The more information you provide in an appeal or re-determination, the better and easier it will be to state the case and get the claim paid.
Prevent Future Medical Billing Errors
To avoid wasting more time and prevent future claim corrections, it is important not to repeat the same errors.
As an example, duplicate claims happen sometimes. These errors are mostly preventable, though.
Therefore, understanding your billing software and developing a plan to make sure the claim only goes out once is paramount to billing efficiency.

Another common error is failing to check if the patient is eligible for coverage for the service date with their insurance plan. Again, it is important to verify eligibility and work out any kinks before sending claims.
Some patients don’t know or understand their coverage (primary, secondary, tertiary). The billing team’s experience, along with eligibility verification, should help determine which insurance gets the claim first.
It is also worth mentioning that coding the claim correctly is of the utmost importance. Designating the correct ICD-10 codes with the correct CPT codes will get your practice paid and avoid any unnecessary questions or audits.
Implementing strategies to help the billing process get claims paid the first time can come with trial and error. However, once common mistakes are identified, a plan can be put in place to prevent them.
Surely, submitting medical claims correctly the first time is the best practice, but correcting claims does not need to be feared.
Get Payment for Your Medical Claims
Getting these medical claims back out for determination and payment quickly and efficiently is key. Don’t waste precious time and money sitting on these claim errors. In short, if you get a claim back due to a mistake, don’t panic.
All you need to do is identify the mistake and fix it. Then, finally, learn from the mistake and fix policy to avoid repeating.
Not sure your practice’s billing services are the best they can be? Get a quote from Medical Billing Service Review for a software upgrade or even entirely new medical billing services.
Author: Mike Cynar
Mike Cynar brings buyers and sellers together by producing reviews and creating non biased webpages allowing users to share their experiences on various products and services. He and his staff write informative articles related to the medical field, legal, and other small business industries.

Leave a Reply