Medical Billing Discussion: Types of Service Codes (Chart)
 What are the different types of service codes for medical billing? Brought to you from Medical Billing Service Review, learn all about the codes so you can be reimbursed for your services without any hassles. See full chart of codes to the right (and snippets below):
What are the different types of service codes for medical billing? Brought to you from Medical Billing Service Review, learn all about the codes so you can be reimbursed for your services without any hassles. See full chart of codes to the right (and snippets below):
Doctors began classifying diseases during a bubonic plague outbreak in 17th-century London. The data collected enabled doctors to track causes and symptoms in the hopes of preventing further deaths.
COMPARE MEDICAL BILLING QUOTESLater coding systems had similar goals. They were also invaluable tools in disease prevention. Doctors worldwide could communicate using medical codes. Countries could also use the codes to track causes of death (as opposed to listing numbers of mortality).

Today, medical codes serve the needs of medical billers. They employ various types of service codes to show how patient’s medical information can be billed properly. Indeed, a good medical biller can increase profits at their institution, and the opposite is also true.
If you are familiar with these codes, you can make sure you are being reimbursed properly.
What are the different types of service codes used by medical billers? Let’s find out!
Transaction Code List – General Type of Service:
01-Medical Care
02-Surgery
03-Consultation
04-Diagnostic X-Ray
05-Diagnostic Lab
06-Radiation Therapy
07-Anesthesia
08-Surgical Assistance
09-Other Medical
10-Blood Charges
11-Used DME
12-DME Purchase
13-ASC Facility
14-Renal Supplies in the Home
15-Alternate Method Dialysis Payment
16-CRD Equipment
17-Pre-Admission Testing
18-DME Rental
19-Pneumonia Vaccine
20-Second Surgical Opinion
21-Third Surgical Opinion
51-Purchased Lab
95-Psychiatric Assistant
97-Room and Board
99-Ancillaries
Transaction Code List – Unique Type of Service:
1G-Global Service Radiology
1H-Global Service Laboratory
A-Ambulance
B-Maternity
BL-Blood/Packed Cells
C-Chiropractic
CB-Cosmetic Surgery-Beautification
CC-Concurrent Care
CS-Cosmetic Surgery-Necessary
D-Occupational Therapy
E-DME-Used Without Warranty
G-Medical Diagnostic Services
GG-Drugs
H-Special Medical Therapeutics
HS-Hospice
I-Dental
II-Professional Component
J-Therapeutic Injections
JJ-Interpretation
K-Monitoring Services
KK-Emergency Care
L-Speech Therapy
LL-Home Care Program
MM-Vision
N-Kidney Donor
NC-60% Non Emergency Consultation
NN-Visiting Nurse Services
What Do Medical Billers Do?
Medical billers collect all relevant patient information and compile it into a bill for the insurance company. This bill is called a claim, and it must have correct diagnostic, service, and revenue codes. They help ensure the insurance company pays the claim.
Medical billers may work alongside a medical coder. Or they may themselves be the coder in addition to performing billing services.
Of course, the coder is responsible for translating patients’ clinical details into code. But the biller must understand all codes in order to process patients’ claims.
Coding can be a complicated process. There are CPT codes, ICD-10 codes, and HCPCS Level I and Level II codes. In the following sections, let’s discuss the types of codes used in billing so you can understand the system better.
COMPARE MEDICAL BILLING QUOTESICD Codes
 A patients’ claim form will have both a diagnostic as well as a procedural code. Applying the correct code to a patient’s diagnosis falls to the medical coder. Yet the biller must also understand the code and make sure it aligns with insurance policies.
A patients’ claim form will have both a diagnostic as well as a procedural code. Applying the correct code to a patient’s diagnosis falls to the medical coder. Yet the biller must also understand the code and make sure it aligns with insurance policies.
Patients’ diagnoses are labeled according to ICD-codes. They were developed by the World Health Organization, and there is a code for every known disease.
ICD codes tell the insurance company why the patient visited the doctor and must be linked properly to the CPT (or diagnostic) code.
Let’s examine those in the next section.
CPT Codes
CPT stands for Current Procedural Terminology. These codes are published by the American Medical Association, and right now there are about 10,000 CPT codes used in the United States.
CPT codes tell the insurance company what services the patient received. These could be medical, surgical, radiological, or diagnostic.

They are submitted on claim forms along with ICD-10 codes. All this information is needed for insurance companies to remit payment either to a provider or an institution.
CPT codes give medical professionals and insurance companies a common language. This is what makes them important. It also simplifies the claims process.
Medical billers, as well as coders, need to know both ICD-10 and CPT codes intimately. Different insurance companies reimburse similar conditions differently.
One insurance company pays a certain amount for a certain code. Another insurance company will pay a different amount for the exact same code. You can see, then, how important a medical biller’s knowledge of the types of bill codes is for financial success.
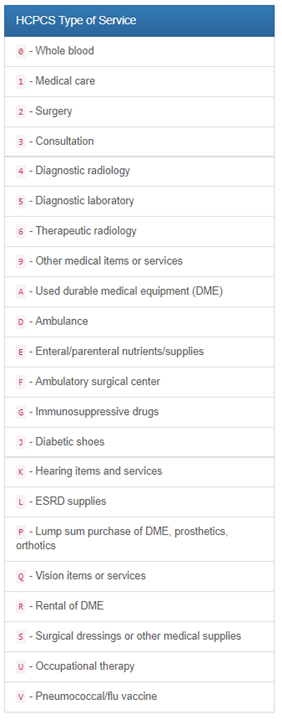
HCPCS Codes
 Medicare, Medicaid, and some other third-party payers require medical billers to use HCPCS codes. Although HCPCS codes are based on CPT codes, it can be difficult for medical billers to know which type of service code to use. That fact helps explain why experienced billers are such assets to medical offices.
Medicare, Medicaid, and some other third-party payers require medical billers to use HCPCS codes. Although HCPCS codes are based on CPT codes, it can be difficult for medical billers to know which type of service code to use. That fact helps explain why experienced billers are such assets to medical offices.
HCPCS was set up in 1978, and, at first, use of these new codes was optional. That changed with the passage of the Health Information and Portability Act (HIPPA) in 1996.
HIPPA standardized coding practices. It mandated that ICD codes be used for diagnosis, while CPT and HSPCS codes were for medical procedures.
Medical billers must follow HIPPA guidelines when submitting their claims. Otherwise, insurance companies will reject them.
HCPCS codes have three levels. Level I codes are the basically the same as CPT codes (even though medical billers refer to them as HCPCS Level I codes).
Level II codes will be discussed below. In general, though, they are codes not found in CPT and refer to products, supplies, and procedures not provided by physicians.
Level III HCPCS codes were developed by state agencies for local areas. They are not recognized at the national level.
HCPCS Codes Level II
HCPCS Level II codes cover medical procedures. Medical billers use them for non-physician services such as:
- ambulance services
- prosthetic devices
- drugs or surgical supplies
- non-physician services that aren’t included in Level I codes (CPT)
HCPCS codes are submitted on a claim form called the CMS-1500.It contains HCPCS as well as other service codes.
One of these other codes is the Type of Service (TOS) code. All HSPCS codes have a corresponding TOS code, just like ICD-10 codes always go with CPT.
TOS codes refer to the procedures or services the patient experienced. It is used mainly to collect data, but it sometimes affects payment.
Another type of service code is the Place of Service (POS) code. This tells the insurance company where the patient received their services. POS codes are maintained by CMS, just like all HCPCS codes are.
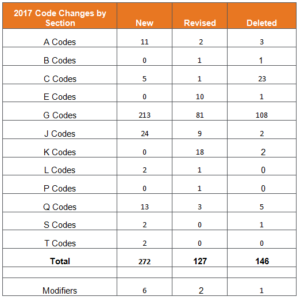
There are many specific guidelines for the use of HCPCS codes. They can be highly detailed, and medical billers need to be aware of any guideline changes or modifications. Significant components like the type of equipment used or the amount of medication cannot be overlooked.
The level of detail required for proper reimbursement is great. A quality medical biller will have the expertise to stay ahead of HCPCS changes and details.
Wrapping Up on the Types of Service Codes
As you can see, there are many types of bill codes that go into making a correct insurance claim. Although medical coders are responsible for the diagnosis codes, the biller needs to understand the various types of service codes and so much more.
Given the complexity of medical billing, you might want to consider hiring a medical billing company. We have the most current information on billing companies, and we can help you find the best one to fit your needs.
Why not contact us today for a quote? We want your medical office to run as smoothly as possible!
COMPARE MEDICAL BILLING QUOTESMaximizing Reimbursements with Accurate Service Code Usage in Medical Billing
Medical billing is a crucial aspect of the healthcare industry, as it ensures that healthcare providers receive proper payment for the services they provide. Service codes play a vital role in the medical billing process, as they determine the amount of reimbursement a healthcare provider will receive for a particular service.
Service codes are standardized codes that describe specific medical procedures or services. They are used by insurance companies and government programs such as Medicare and Medicaid to determine the amount of reimbursement a healthcare provider will receive for a particular service. The accuracy of service codes is essential to ensure that healthcare providers receive the proper amount of reimbursement for their services.
Using the Correct Service Code
One of the biggest challenges in medical billing is the selection of the correct service code for each procedure or service provided. Choosing the wrong service code can result in denied claims, reduced reimbursements, and even fines from government agencies. To maximize reimbursements, it is crucial to have a thorough understanding of service codes and the proper way to use them in medical billing.
One way to improve the accuracy of service codes is to stay up-to-date with the latest codes and changes. The Centers for Medicare and Medicaid Services (CMS) regularly updates the codes used for medical billing, so it is important to stay informed about any changes that may impact the reimbursement process.
Medical Billing Systems
Another way to ensure accurate service code usage is to have a robust medical billing system in place. A well-designed medical billing system can help healthcare providers efficiently manage their billing processes and reduce the likelihood of errors or omissions. It can also provide real-time feedback on the accuracy of service codes and help providers avoid common mistakes that can result in denied claims.
In addition to having a robust medical billing system, it is also important to have a well-trained medical billing team. A team that is knowledgeable about service codes and the medical billing process can help ensure that claims are submitted accurately and in a timely manner, resulting in faster reimbursements and fewer denied claims.
An accurate service code usage is essential to maximizing reimbursements in medical billing. By staying informed about the latest changes, implementing a robust medical billing system, and having a well-trained medical billing team, healthcare providers can ensure that they receive the proper reimbursement for their services and minimize the risk of denied claims or reduced reimbursements.
The Future of Service Codes in Medical Billing: Trends and Predictions
Service codes play a crucial role in the medical billing process, as they determine the amount of reimbursement a healthcare provider will receive for a particular service. With the rapid advancement of technology in the healthcare industry, the future of service codes in medical billing is likely to change. Here are some of the trends and predictions for the future of service codes in medical billing:
- Increased Use of Electronic Health Records (EHRs): The use of electronic health records (EHRs) is expected to increase in the coming years, as healthcare providers adopt digital systems to manage their patient data. This will likely result in a more streamlined medical billing process, as service codes will be automatically populated into EHRs, reducing the likelihood of errors and improving the accuracy of billing.
- Shift to Value-Based Care: The shift to value-based care is expected to impact the way service codes are used in medical billing. Under value-based care, healthcare providers are paid based on the quality of care they provide, rather than the volume of services they perform. This means that service codes will need to be more comprehensive and accurately reflect the quality of care provided.
- Increased Focus on Data Analytics: Data analytics is becoming increasingly important in the healthcare industry, as it helps providers understand patient needs and improve the quality of care. In the future, service codes may be used to collect data on patient outcomes and treatment effectiveness, allowing providers to better understand the impact of their services and make improvements where necessary.
- Standardization of Service Codes: The standardization of service codes is likely to become even more important in the future, as healthcare providers seek to improve the accuracy of billing and reduce the risk of denied claims. By using standardized codes, healthcare providers can ensure that they receive the proper reimbursement for their services and minimize the impact of coding errors on their bottom line.
In conclusion, the future of service codes in medical billing is likely to be impacted by the increasing use of technology, the shift to value-based care, the increased focus on data analytics, and the standardization of codes. By staying informed about these trends and predictions, healthcare providers can ensure that they are prepared for the future of medical billing and continue to receive proper reimbursement for their services.
COMPARE MEDICAL BILLING QUOTESAuthor: Mike Cynar
Mike Cynar brings buyers and sellers together by producing reviews and creating non biased webpages allowing users to share their experiences on various products and services. He and his staff write informative articles related to the medical field, legal, and other small business industries.
Leave a Reply